
What is Diabetic Retinopathy?
Diabetic Retinopathy (DR) is an ocular complication of Type 1 and Type 2 Diabetes Mellitus. This complication may develop several years after the onset of diabetes. It is one of the leading causes of blindness in adults of productive age (20-70 years).
If you have diabetes, this means that your body is not using and storing sugar properly. High blood sugar levels can cause damage to the blood vessels of the retina - the nerve layer at the back of the eye that perceives light and helps send images to the brain. This damage to the retinal vessels and the retina is called Diabetic Retinopathy.
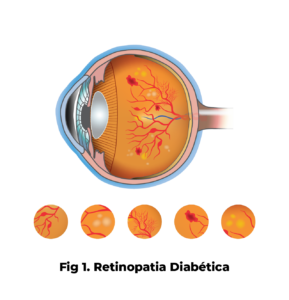
Fig.1: Diabetic Retinopathy
Fluorescein angiography
Early detection of diabetic retinopathy results in better protection against vision loss and today, due to more advanced methods of diagnosis and treatment, only a small percentage of people who develop diabetic retinopathy have serious vision problems.
PREVENTION
Prevention being one of the predominant factors in reducing the long-term risk of vision loss, it is fundamental to comply with some basic rules in order to delay the appearance of DR or to avoid its aggravation. These are:
- Have an annual ophthalmology consultation;
- Carry out a metabolic control of diabetes, namely to comply with the pharmacological treatment plan, the diet and exercise plan. It is also extremely important to control arterial hypertension, cholesterol, triglycerides and renal function.
SYMPTOMS
In diabetic retinopathy the symptoms vary according to the stage of the disease. In an initial phase, it is asymptomatic, hence the importance of an annual consultation. As the disease progresses, the patient notices blurred vision, one of the most frequent symptoms, which becomes worse.
When to book an examination?
By keeping a close watch on your blood sugar level and seeing an ophthalmologist regularly you can significantly reduce the risk of sight loss.
Right after the first diagnosis of diabetes, you should have an eye examination:
- Within five years of diagnosis if you have type 1 diabetes;
- Soon after diagnosis if you have type 2 diabetes (usually diagnosed after the age of 30).
People with diabetes should schedule dilated eye examinations at least once a year. More frequent examinations by an ophthalmologist may be necessary after diabetic retinopathy has been diagnosed.
It is recommended that pregnant women with diabetes make an appointment in the first trimester because retinopathy can progress rapidly during pregnancy.
If you need an eye examination you must remember that your blood sugar level should be under regular control for a few days before you go to the optician. Spectacles that work well when your blood sugar is out of control do not work well when the sugar content is stable.
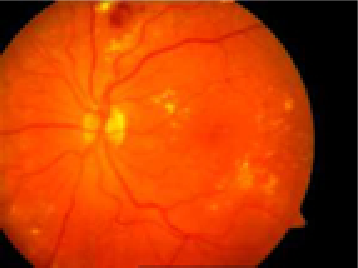
Fig.2: Diabetic retinopathy
Types of Diabetic Retinopathy
There are two types of diabetic retinopathy: non-proliferative diabetic retinopathy (NDRP- fig.1 and 2 - see previous explanation) and proliferative diabetic retinopathy (PDR- fig.3).
PNDR, or non-proliferative diabetic retinopathy, is a phase of the disease in which the retinal vessels leak blood or fluid (fig.1 and 2). These cause the retina to swell (retinal oedema) and lead to the formation of deposits (hard exudates). At the same time, these blood vessels can progressively close and the retina can become bloodless (ischaemia). When oedema or ischaemia affects the macula - the central part of the retina responsible for detailed vision, such as reading or sewing - vision is affected.
Fig.3: Fluorescein angiography
Proliferative Diabetic Retinopathy
-Macular oedema is a thickening of the macula, a small area in the centre of the retina that allows us to see detail clearly. The thickening is caused by fluid passing from the blood vessels in the retina. It is the most common cause of visual loss due to diabetes. The vision loss can be moderate or severe, but even in the worst cases, peripheral vision continues to function.
- Macular ischaemia occurs when small blood vessels (capillaries) close. Vision becomes blurred because the macula does not receive enough blood to function well. (Fig 3)
PDR, or proliferative diabetic retinopathy, presents when new abnormal vessels (neovascularisation) begin to grow on the surface of the retina or optic nerve. The primary cause of PDR is extensive occlusion (closure) of retinal blood vessels, thus preventing adequate blood flow. The retina responds by generating new blood vessels in an attempt to supply blood to the area where the original vessels have closed (Fig 4).
Unfortunately our abnormal blood vessels do not replenish the retina with normal blood flow and often these new vessels are accompanied by scar tissue which can cause wrinkling or detachment of the retina.
PDR can lead to more severe visual loss than PNDR as it affects both central and peripheral vision.
Proliferative diabetic retinopathy causes vision loss in several ways:
- Vitreous haemorrhage: New, fragile vessels can bleed into the vitreous, a clear, jelly-like substance that lines the centre of the eye. If the vitreous haemorrhage is small, the person may see only a few new, dark floaters. A very large haemorrhage can completely obstruct vision. It may take days, months or even years to reabsorb the blood, depending on how much of it is present. If the eye does not eliminate the blood properly within a reasonable time, surgery (vitrectomy) may be the recommended solution to remove it.
Fig.4: Fluorescein angiography
Proliferative Diabetic Retinopathy
CONTACTS
COIMBRA
Espaço Médico de Coimbra
Rua Câmara Pestana, n.º 35-37
3030-163 Coimbra, Portugal
Phone: +351 239 484 348 /Telm: +351 966 320 022
Fax: +351 239 481 487
E-mail: emc@oftalmologia.co.pt
AVEIRO
Rufino Silva - Clínica Oftalmológica
Av. Lourenço Peixinho, Nº 177-179, 2º andar
3800 - 167 - Aveiro
Tel: +351 234 382 847
Mobile: +351 918 644 767
E-mail: aveiro@oftalmologia.co.pt
FORM
COIMBRA
Espaço Médico de Coimbra
Rua Câmara Pestana, n.º 35-37
3030-163 Coimbra, Portugal
Phone: +351 239 484 348 /Telm: +351 966 320 022
Fax: +351 239 481 487
E-mail: emc@oftalmologia.co.pt
AVEIRO
Rufino Silva - Clínica Oftalmológica
Av. Lourenço Peixinho, Nº 177-179, 2º andar
3800 - 167 - Aveiro
Phone: +351 234 382 847
Mobile: +351 918 644 767
E-mail: aveiro@oftalmologia.co.pt
COIMBRA
Espaço Médico de Coimbra
Rua Câmara Pestana, n.º 35-37
3030-163 Coimbra, Portugal
Phone: +351 239 484 348 /Telm: +351 966 320 022
Fax: +351 239 481 487
E-mail: emc@oftalmologia.co.pt
AVEIRO
Rufino Silva - Clínica Oftalmológica
Av. Lourenço Peixinho, Nº 177-179, 2º andar
3800 - 167 - Aveiro
Phone: +351 234 382 847
Mobile: +351 918 644 767
E-mail: aveiro@oftalmologia.co.pt

