PUBLIC AND PATIENTS
Age-related Macular Degeneration (AMD)
WHAT IS age-related macular degeneration (AMD)?
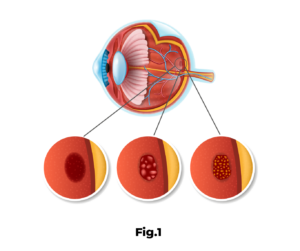
Age-related Macular Degeneration (AMD), in its most severe form, the exudative or wet form, is characterised by the growth of abnormal blood vessels behind the retina, also called choroidal neovascular membrane or choroidal neovessels that cause the retina to appear swollen and haemorrhagic. Without treatment, the vast majority of patients develop a scar in the centre of the macula and suffer severe vision loss. People affected in both eyes cannot read, sew or drive and have enormous difficulties in their daily activities. They feel highly limited in carrying out such routine tasks as telling the time or dialling a telephone number. It is estimated that in Portugal there are around 2500 to 3000 new cases of this disease every year.
SYMPTOMS
In AMD. there is damage to the macula, a small area at the back of the eye that allows you to see small details clearly. When the macula does not function properly, the patient cannot, for example, read, drive or correctly identify a face.
Age macular degeneration alone does not result in total blindness, although it reduces vision in the central part of the retina, it does not impair the lateral, or peripheral vision of the eye. The patient can see the outline of a clock, but cannot see the time.
CAUSES
MOST COMMON TYPES OF AMD
There are two most common types of AMD: the atrophic form and the exudative form.
ATROPHIC DMI:
Most people have atrophic AMD. This accounts for 80-90% of all AMD cases and is responsible for about 10-20% of all cases of marked vision loss. Vision loss is usually slow.
EXUDATIVE DMI:
Exudative AMD accounts for only 10-20% of all AMD cases. It accounts for 80-90% of cases of marked vision loss. It results from the formation of new blood vessels at the bottom of the eye (neovessels). These new blood vessels leak fluid or blood and cause the loss of detailed vision, such as watching TV or distinguishing faces. The loss of vision can be rapid and severe.
SYMPTOMS
What are the symptoms of AMD?
Atrophic or dry AMD can remain almost unnoticed by the patient for many years or may even be symptomless. The exudative form is much more serious. The patient may notice distorted images and lose reading vision in one eye within a few days. When both eyes are affected, loss of central vision can be seen more quickly.
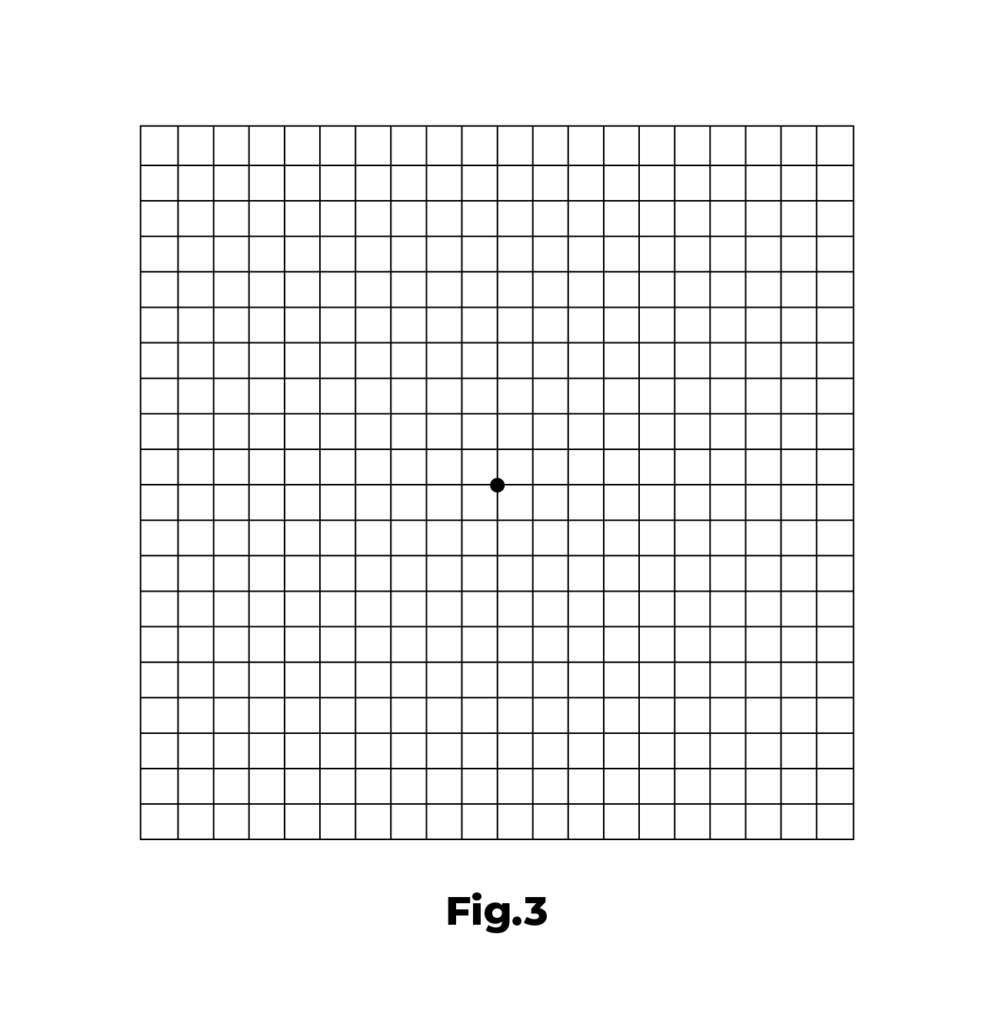
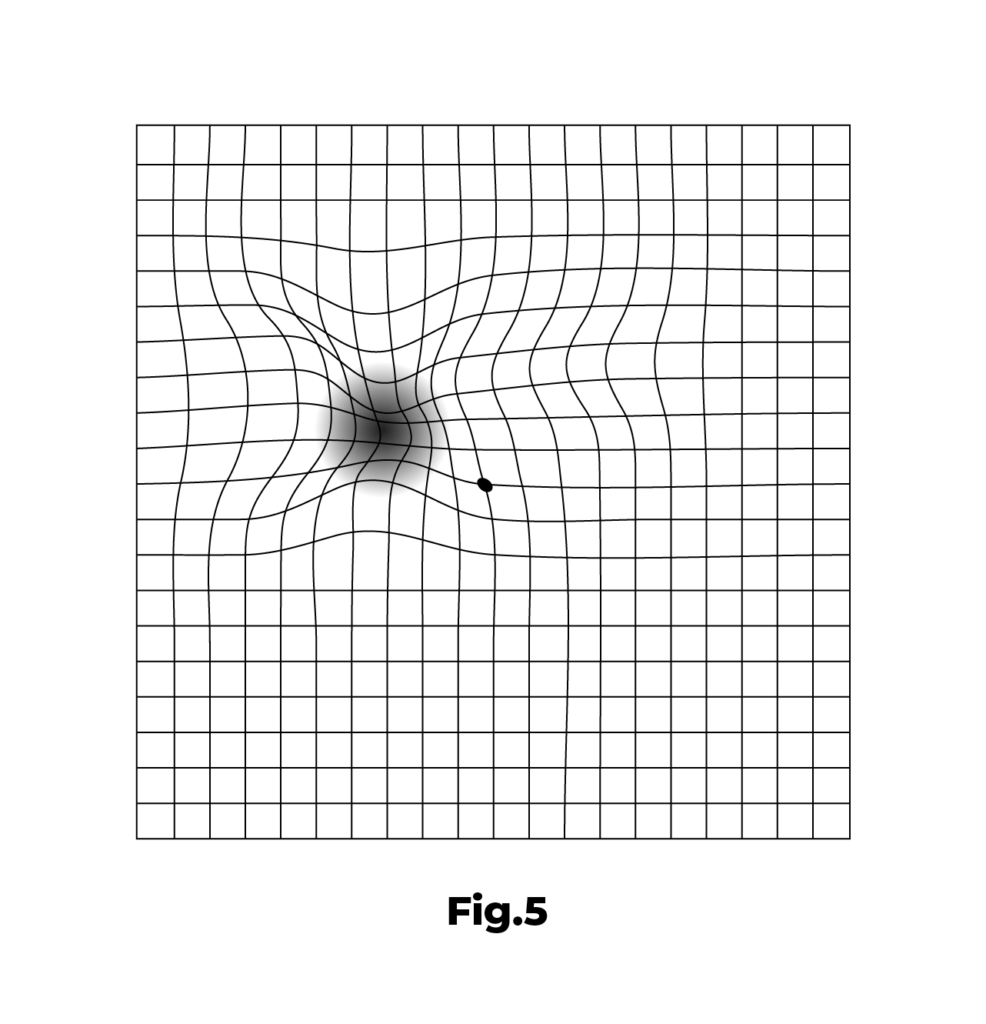
How can the patient detect vision loss? The Amsler Grid
- in the centre of the vision a dark or empty area appears;
- the straight lines appear crooked, as in the diaphragm below:
AMSLER GRID
Test your eyesight with the Amsler grid:
You can test your eyesight every day using an Amsler grid like the one below. You may notice changes in your vision that would otherwise be unnoticeable. Place the grid on your refrigerator door and test daily, especially if you are over 65 or if your doctor has recommended you to do so.
To use the Amsler grid:
- Put on your reading glasses and hold this grid at a distance of 30-45 centimetres, in good light.
- Cover one eye. Look directly at the point in the centre with your eye uncovered.
- While looking directly at the point in the centre, notice if all the lines of the grid are straight or if any areas look crooked, blurred or dark. Repeat this procedure with the other eye.
- If any area of the grid looks wavy, blurred or dark, contact your eye doctor immediately.
DIAGNOSTICS
How is AMD diagnosed?
Many people don't know they have any macular problems until distorted vision or a shadow that doesn't disappear from the central field of vision becomes evident.
Your ophthalmologist can detect the first signs of ARMD during your consultation by:
- Looking at the macula with an ophthalmoscope;
- A very simple test with a grid;
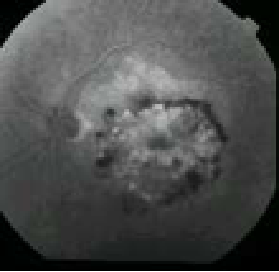
- Additional tests such as OCT or angiography to locate the abnormal blood vessels under the retina. One or two fluorescent dyes (fluorescein and indocyanine green) are injected into a vein in the arm and photographs are taken as the dye passes through the blood vessels deep in the eye.
CONTACTS
COIMBRA
Espaço Médico de Coimbra
Rua Câmara Pestana, n.º 35-37
3030-163 Coimbra, Portugal
Phone: +351 239 484 348 /Telm: +351 966 320 022
Fax: +351 239 481 487
E-mail: emc@oftalmologia.co.pt
AVEIRO
Rufino Silva - Clínica Oftalmológica
Av. Lourenço Peixinho, Nº 177-179, 2º andar
3800 - 167 - Aveiro
Tel: +351 234 382 847
Mobile: +351 918 644 767
E-mail: aveiro@oftalmologia.co.pt
FORM
COIMBRA
Espaço Médico de Coimbra
Rua Câmara Pestana, n.º 35-37
3030-163 Coimbra, Portugal
Phone: +351 239 484 348 /Telm: +351 966 320 022
Fax: +351 239 481 487
E-mail: emc@oftalmologia.co.pt
AVEIRO
Rufino Silva - Clínica Oftalmológica
Av. Lourenço Peixinho, Nº 177-179, 2º andar
3800 - 167 - Aveiro
Phone: +351 234 382 847
Mobile: +351 918 644 767
E-mail: aveiro@oftalmologia.co.pt
COIMBRA
Espaço Médico de Coimbra
Rua Câmara Pestana, n.º 35-37
3030-163 Coimbra, Portugal
Phone: +351 239 484 348 /Telm: +351 966 320 022
Fax: +351 239 481 487
E-mail: emc@oftalmologia.co.pt
AVEIRO
Rufino Silva - Clínica Oftalmológica
Av. Lourenço Peixinho, Nº 177-179, 2º andar
3800 - 167 - Aveiro
Phone: +351 234 382 847
Mobile: +351 918 644 767
E-mail: aveiro@oftalmologia.co.pt

